History
Who we are
“If there was ever a Christ-like work in the world, it is to go amongst these poor sufferers and bring them the consolation of the gospel.”—Wellesley Bailey
Wellesley Bailey, the founder of The Leprosy Mission, said this after he saw first-hand the appalling living conditions and social isolation of people suffering from leprosy in 1869.
It wasn’t until 1913 when Bailey and his wife Alice visited Australia that he inspired locals to found their very own support chapter.
The Leprosy Mission Australia was formed to raise awareness about leprosy and provide financial support to bring hope and healing to people affected by the disease.
-
1860s

A general view of the Leprosy Asylum at Ambala (circa 1900; 40 years after Wellesley commenced work there)
In 1869, Wellesley was teaching at a mission school in Ambala, India. The school principal, Dr Morrison, invited him to visit a small leprosy asylum. The experiences of the people there inspired Wellesley to commit to regular visits. During his work in Ambala, he wrote regularly to his childhood friend, Alice Graham. It was in this correspondence that they became engaged. Wellesley Bailey also shared stories from the Ambala leprosy asylum which Alice would pass on to her friends, the Pim sisters.
-
1870s
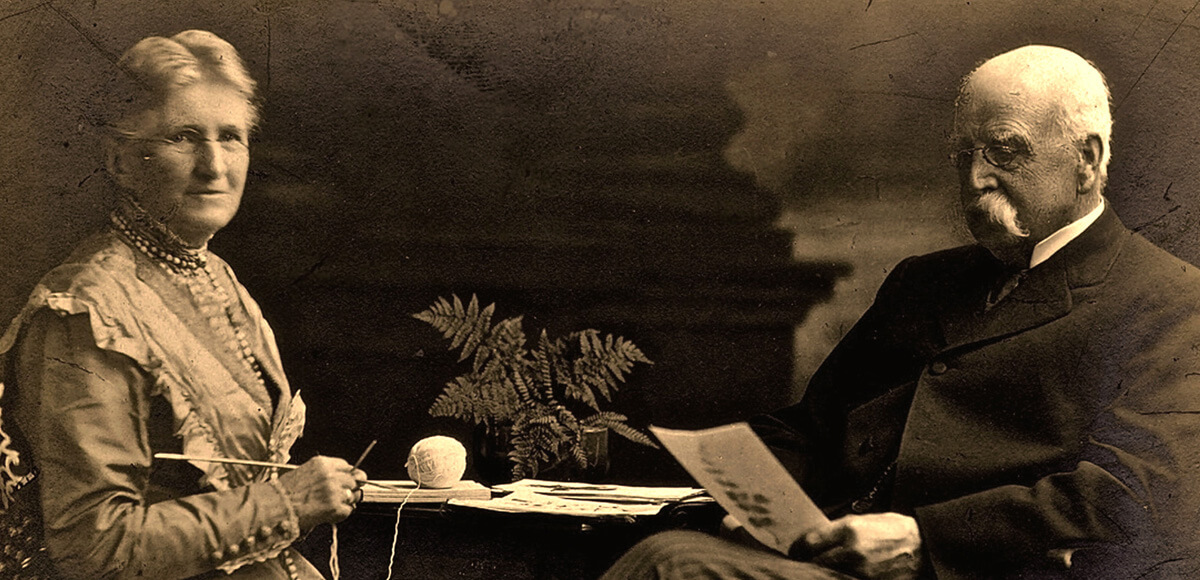
Alice and Wellesley Bailey
Alice married Wellesley in India in 1871. Three years later, they returned to their native Ireland. Their childhood friends, the Pim sisters, encouraged them to speak of their work at the Ambala Leprosy asylum. Following a meeting in their house, the Pim sisters arranged a more public address at the Monkstown Quaker Meeting House. A tract from this address was circulated throughout Dublin. Four years later, in 1878, “The Mission to Lepers” was formalised (which was later renamed “The Leprosy Mission”). In 1873, the Norwegian physician Gerhard Armauer Hansen identified the bacteria responsible for leprosy. He named it M.leprae. Dr Albert Neisser stained the bacteria, improving its identification seven years later.
-
1890s

Portrait of Mary Reed, written on the backdrop is “My times are in Thy hand” and above its frame is written “My grace is sufficient for thee” (circa 1908)
In 1891, Mary Reed became The Leprosy Mission’s first missionary. She was appointed to work in a leprosy asylum in Chandag, Northern India. After contracting leprosy herself some years prior, she was miraculously cured. She helped build a church, chapels and a small hospital, improved housing and arranged a well to bring safe water into the village.
-
1900s

Sandhlu, a woman affected by leprosy in Chamba, India (circa 1912)
Reverend J. A. Cullen, the first honorary superintendent for The Leprosy Mission in India, visited Melbourne following some ill health. An enthusiastic churchman and bank manager Horace J. Hannah invited him to make an address to the Gleaner’s Union at Holy Trinity Church. A donation of 2 pounds and 10 shillings was collected for people affected by leprosy. Correspondence and support continued, largely through the efforts of Hannah, for the next ten years. In 1908, Hannah and his friends established an auxiliary.
-
1910s

Wellesley Bailey and his wife travel to China, Australia, New Zealand, the Philippines, Japan, Korea, Malaysia, Singapore and India, visiting projects, raising awareness of leprosy and asking for support.
It wasn’t until a visit by Wellesley and Alice Bailey in 1913, that Australians decided to formally establish their own The Leprosy Mission chapter. On 8 July a meeting was held in the Church Missionary Association Reading Room in Melbourne. Twenty people joined together, various positions were appointed (Hannah was appointed Honorary Secretary and Treasurer), and The Leprosy Mission Australia was formally founded. A couple of months later, Hannah was formally appointed President and Honorary Treasurer, positions he held until he died in October 1958. On the brink of war, it would be a difficult next few years. Yet The Leprosy Mission flourished. By the time Wellesley Bailey retired in 1917 The Leprosy Mission had 87 programmes in 12 countries and support offices in eight countries.
-
1920s
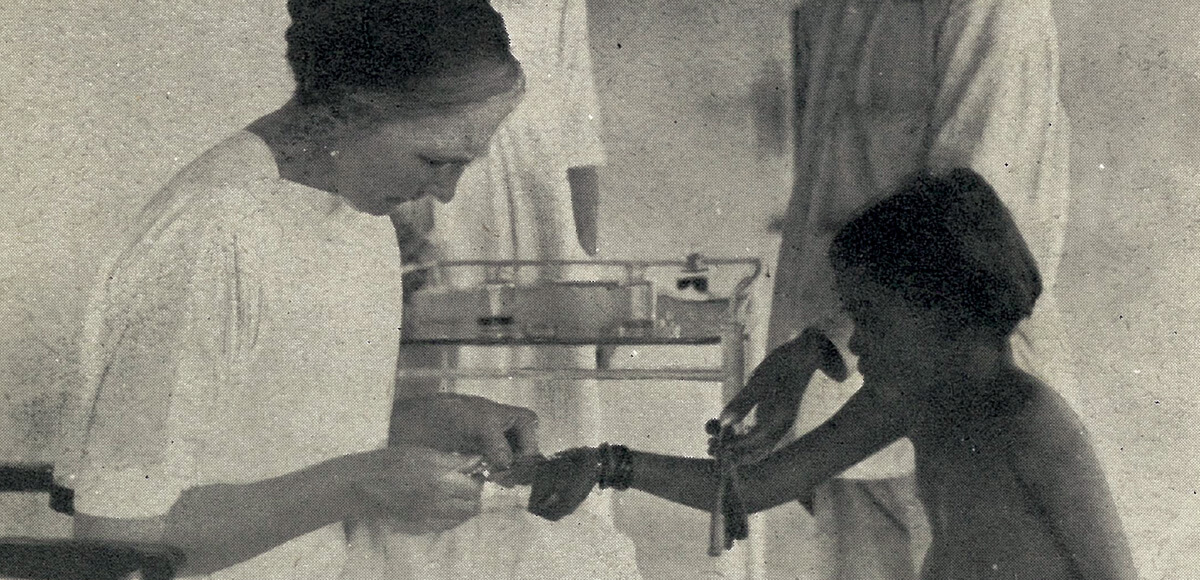
Dr Isabel Kerr giving an injection (most probably chaulmoogra oil) to an Indian girl affected by leprosy (circa 1924)
Following great advances in microbiology over the last fifty years, a treatment for leprosy had become available. Patients received oil derived from the Chaulmoogra tree to be taken orally or injected into the skin. Some people were cured in this way. With a flush of hope, the word “asylum” was outlawed in 1925, and replaced with “hospital” and its promise of healing. The Leprosy Mission’s headquarters moved from Dublin to London and a bold aim to eradicate leprosy was adopted, focussing at least partly on the additional benefits of improving living conditions.
-
1930’s
In 1935 the powerful antibiotic drug “DDS” (short for “Diamino-Diphenyl-Sulphone”) was developed. Initially three German chemists had discovered the compounds in 1908. Yet it did not suit their purposes and was shelved. It was later developed by several chemists during the 1930s, and earned one of them a Nobel prize. Initial trials proved that the drug was too toxic and too expensive as an antibiotic. But refinements in production eventually resulted in the drug known as Dapsone.
Hospitals began to replace leprosy “asylums”; the work expanded into Africa, Asia, and the Far East. The Mission’s headquarters moved from Dublin to London. The bold aim to eradicate leprosy was adopted.
-
1940’s

Dr Paul Brand and Dr Stanley Browne share their expertise in Karigiri (circa 1950)
The world had returned to war and The Leprosy Mission’s work was severely disrupted. Many patients were dispersed, hospitals were destroyed or abandoned, and staff interred. Immediately following the War, great medical advances were made.
Dr Paul Brand, who later joined The Leprosy Mission, introduced the view that the loss of fingers and toes was due to infection and thus wholly preventable. Drawing upon his experiences as an orthopaedic surgeon during the war, he pioneered “tendon transfer” surgery with his colleagues in Karigiri, India to correct leprosy-related deformities.
Dr Margaret Brand, his wife, devoted herself to preventing blindness in people affected by leprosy. These advances would also prove invaluable for people with diabetes and other diseases.
In 1945, the first effective cure for leprosy, Dapsone, became available.
-
1950’s

Fransciscan Missionaries of Mary serve the population at the Fantone Island leprosarium in Australia. It closed in 1973.
Following the release of Dapsone, millions of patients were successfully cured and many leprosy colonies, no longer relevant, were closed.
Some strains of leprosy begin to develop a resistance to the drug.
A year later, a researcher identified Clofazimine as an effective drug against leprosy. Clofazimine would later join Dapsone and one other drug as the modern cure used universally today.
-
1960’s
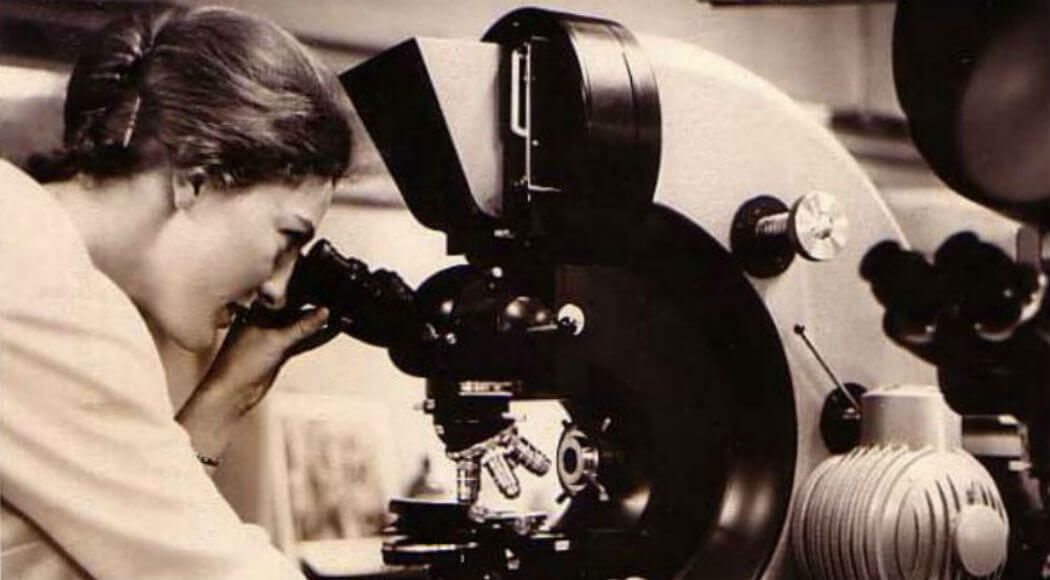
In 1962, microbiologist Mary, dreamed of becoming a medical missionary, eventually serving at The Leprosy Mission in Australia and the UK.
In 1960, leprosy was successfully transmitted to mouse footpads for laboratory testing. Seven years later this resulted in the discovery of Rifampicin as an effective antibiotic for leprosy. In 1965, “The Mission to Lepers” formally adopted the new name “The Leprosy Mission” to avoid perpetuating the stigma associated with “leper”.
The Leprosy Mission Australia starts supporting projects in Papua New Guinea, Thailand and Nepal, where the new Anandaban hospital is opened.
The Leprosy Mission’s community work dramatically increased during this period. Local medical staff travelled from village to village finding new cases and providing anti-leprosy drugs under the integrated, patient-centred approach of “Survey, Education, Treatment”.
In 1969, Trevor and Heather Smith began work at the McKean Rehabilitation Centre in Chiang Mai, Thailand.
The quarterly publication “Without the Camp” that began in 1915 was replaced with ACTION Magazine from 1967 and continues today.
-
1970’s

Control work in the Papua New Guinean bush (circa 1965).
By the end of the 1960s, the only fully-tested anti-leprosy drug was ineffective against resistant strains of bacteria. It was becoming increasingly obvious that the wonder-drug Dapsone was becoming unsustainable. Trials that combined multiple treatments for leprosy were carried out.
An estimated 15 million people worldwide still suffering from leprosy, with only one sufferer in every five receiving any sort of treatment.
In response, The Leprosy Mission’s community work dramatically increased; local skilled medical staff travelled from village to village diagnosing new cases and providing anti-leprosy drugs.
-
1980’s

In 1989 TLM staff in Thailand met the Umbrella Girl, whose smile could not be wiped away, even by leprosy.
In 1981, the World Health Organisation (WHO) recommended a new drug treatment for leprosy called Multi-Drug Therapy (MDT). This combination of Dapsone, Clofazimine and Rifampicin drew upon decades of medical research. People could now be cured of leprosy in as little as six months, with almost no risk of antibiotic resistance.
The following year, The Leprosy Mission agreed to adopt MDT in its treatment of leprosy.
As more leprosy-affected people were cured, caring for people with lasting disabilities became increasingly important.
The Leprosy Mission began a programme of social, economic, and physical rehabilitation, and started supporting projects in Nigeria.
-
1990’s
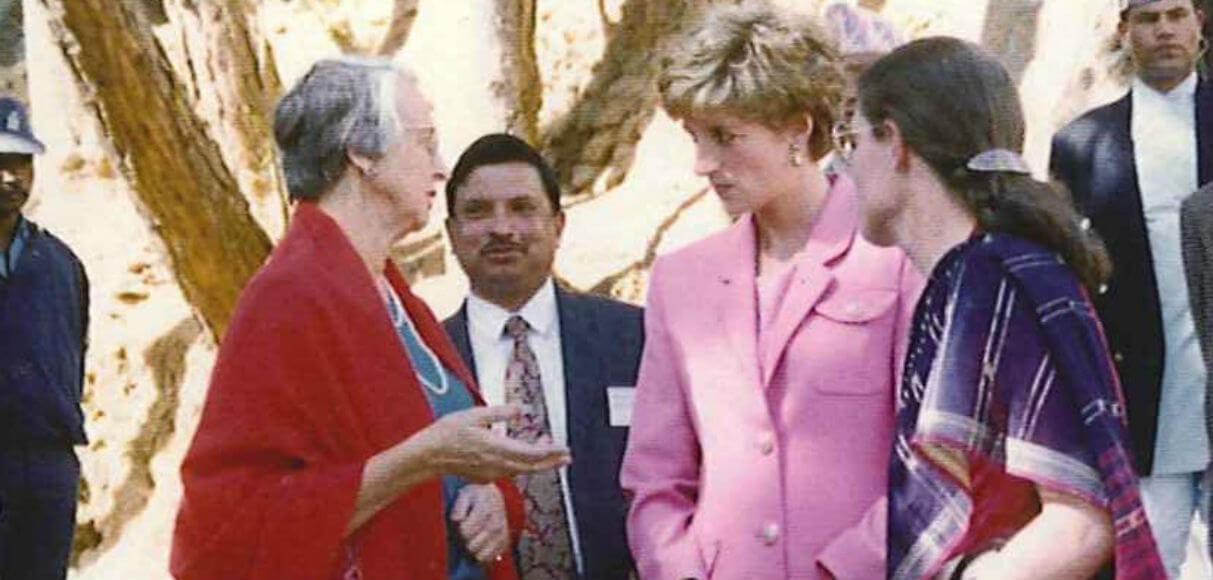
Dr Grace Warren meeting Diana, Princess of Wales, Anandaban Hospital, Nepal, 1993.
Not every country could afford to adopt the use of MDT. But by 1999, the pharmaceutical producers of Clofazimine and Rifampicin, Norvartis, and the Novartis Foundation for Sustainable Development signed an agreement with the World Health Organisation (WHO) to cover the costs of producing and shipping MDT to endemic countries for the next five years. This first agreement has since been extended and expanded in scope, and continues today. The Leprosy Mission Australia began its funding of projects in Timor Leste.
-
2000’s

Sundaram from India lost his boat and livelihood after the 2004 Tsunami but received a boat from supporters (circa 2008).
At the turn of the century, there were significantly fewer cases of leprosy than at any other time in human history. The focus of The Leprosy Mission’s work shifted to training, skills development, and income generation for people affected by leprosy.
In 2008, a second bacteria responsible for leprosy was discovered and given the name M.lepromatosis.
-
2010s

Long-time supporter, Tom, delivering hand-knitted items from Australia to a village in Nepal.
The Leprosy Mission Australia is still committed to the vision of a world without leprosy.
Your support allows expert care to leprosy-affected people to continue throughout the world, restoring individuals, families and communities to a life of hope.